ID’s recommended reads – 10/11/2020 – Laura Van den Borre
The global outbreak of COVID-19 entails large societal and public health challenges. The health impact of the pandemic is not limited to the direct consequences of COVID-19 illness and death: the pressure on health systems and the unprecedented containment policy measures may cause indirect health impacts on multiple dimensions.
The multidimensional health impact of COVID-19 can be decomposed in four dimensions that are portrayed in this figure.
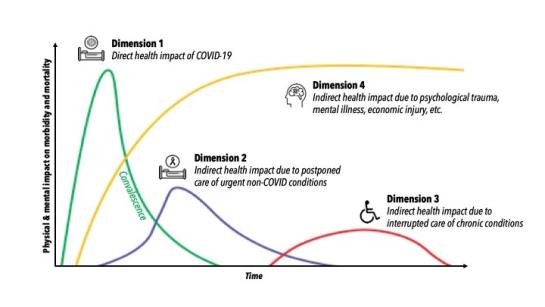
The first dimension considers the direct immediate impact of COVID-19 on public health (e.g. COVID-19 hospitalizations) with the recovery and complications after a COVID-19 infection. The second dimension relates to the impact of postponing urgent primary and hospital care for non-COVID health conditions (e.g. stroke). The third dimension considers the impact of interrupted care for chronic conditions (e.g. cancer) that only gradually becomes apparent. The fourth dimension looks into the impact of mental health challenges and social and economic injury. These health effects can become visible very soon after the outbreak, but it is also possible that they emerge only years later.
Although the overall impact of the COVID-19 crisis on population health can only be fully evaluated with the wisdom of hindsight, knowledge of the short-term and mid-term developments per health dimension is crucial for the further management of the pandemic. The following recommended reads provide valuable insights per health dimension and underline the importance of a multidimensional health perspective.
Dimension 1: The direct health impact of COVID
Risk of COVID-19 among front-line health-care workers and the general community: A prospective cohort study. Nguyen, L. H. et. al (2020).
Nguyen and colleagues focus on the direct immediate health impact on health care workers. This large prospective observational study finds increased infection risk among front-line health-care workers compared to the general population in the United Kingdom and the United States of America. The study identifies an especially vulnerable group: Black, Asian and minority ethnic health-care workers are five times more likely to report a COVID-19 infection, compared to the non-Hispanic white general community. Results seem to suggest that this group is more likely to work in the most at-risk clinical settings. This study also shows a protective effect of the (self-reported) adequacy of personal protective equipment. Although the study population was not randomly selected and further bias may have been introduced by the smartphone driven data collection, this methodologically sound article demonstrates the importance of personal protective equipment and additional targeted policy actions for vulnerable groups in high-risk clinical settings.
Post intensive care syndrome in the aftermath of COVID-19. Hanquet, G. et. al (2020).
Hanquet and colleagues address an expected direct long-term health effect of the COVID-19 crisis. This report provides an overview of the available literature on Post-Intensive Care Syndrome (PICS) and the potential for COVID-19 hospitalized patients to develop this condition. PICS is a wide concept for the physical, cognitive, or mental health impairments arising after critical illness and persisting beyond acute care hospitalization. From a public health perspective, this document provides valuable insights in how to manage the “crisis after the crisis” in Belgium. From a medical perspective, it provides an extensive overview of the literature, detailed contextualization of the Belgian situation, and the practical tools to help PICS patients.
Dimension 2: The indirect health impact due to postponed care of urgent non-COVID-19 conditions
Impact of the COVID-19 outbreak on acute stroke care. Rinkel, L. A. et. al (2020).
The study by Rinkel and colleagues is based on a relatively small study population in the Netherlands but provides very interesting results for the management of non-COVID-19 diseases during the pandemic. The authors compare acute cardiovascular conditions over a 7-week period in the fall of 2019 (pre-pandemic) and in the spring of 2020 (pandemic). Results show a 24% decrease in stroke incidence during the COVID-19 crisis. In addition, the proportion of male stroke patients was higher during the pandemic. Potential explanations include unrecognized symptoms and fear of caregiver transmission. Suggested explanations for the sex differences in stroke incidence during the COVID-19 crisis include a differential impact of the containment measures, as well a sex differences in the disease process of stroke.
Dimension 3: The indirect health impact due to interrupted care of chronic conditions
The impact of the COVID-19 pandemic on cancer deaths due to delays in diagnosis in England, UK: A national, population-based, modelling study.
Maringe, C., et. al (2020).
Maringe and colleagues estimate the indirect mid-term and long-term health effects of interrupted cancer diagnostic pathways and the subsequent delays in cancer diagnoses during the COVID-19 pandemic. This study builds on pre-pandemic individual-level health records with information on referral pathways and diagnostic stage for breast, colorectal, lung and esophageal cancer. These data were linked with expected mortality probabilities, calculated by demographic characteristics using general population life tables.
Even though the effects of suboptimal or delayed cancer treatment have not been investigated, these conservative estimates paint a bleak picture for all three scenarios of diagnostic delay. Compared to the pre-pandemic situation, the United Kingdom is expected to face a 15.3-16.6% increase in colorectal cancer deaths, a 7.9–9.6% increase in breast cancer deaths, a 5.8–6.0% increase in oesophagal cancer deaths, and a 4.8–5.3% in lung cancer deaths up to 5 years after diagnosis. These findings demonstrate the urgent need to maintain routine healthcare services for chronic conditions during the pandemic in order to prevent additional victims of the COVID-19 crisis.
Dimension 4: The indirect health impact due to psychological trauma, mental illness and economic injury.
Derde COVID-19 gezondheidsenquête: Eerste resultaten. Demarest, S., Braekman, E., Charafeddine, R., Drieskens, S., Gisle, L., Hermans, L., & Vandevijvere, S. (2020).
The report of the third COVID-19 health interview survey provides a clear perspective on the mental health challenge and socio-economic hardships in Belgium during the COVID-19 pandemic. The Belgian scientific institute for public health, Sciensano, reached 34,000 adult persons in this third round of the survey. Results show that the prevalence of anxiety disorders (16%) and depressive disorders (15%) is less than determined in the first COVID-19 health survey, but still higher than before the corona crisis (11% and 10% respectively in 2018). Mental health challenges are associated with living alone or in a single-parent family, receiving social security benefits and experiencing financial losses over the last three months. 8% of the respondents report to have considered committing suicide the last three months. In comparison, the 2018 Belgian health interview survey shows 4% of respondents reported thinking about committing suicide the past 12 months. The report further expects that the high state of alertness related to stress during the COVID-19 will lead to exhaustion in the long run.

